What is Ulnar Nerve Entrapment?
Ulnar nerve entrapment is also called cubital tunnel syndrome and ulnar tunnel syndrome. It's the second most common nerve entrapment after carpal tunnel syndrome. It can cause numbness, tingling and/or pain in the arm and certain fingers. The condition is caused by compression or irritation of the ulnar nerve.
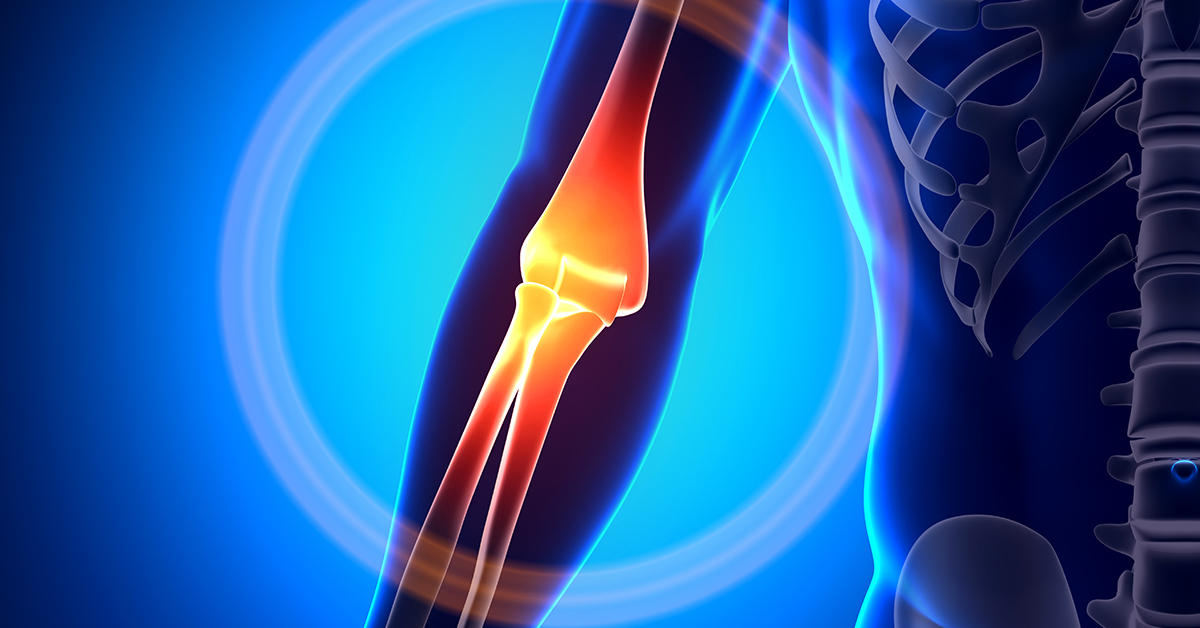
The ulnar nerve travels from the shoulder, down the arm and into the hand. It controls the movement and sensations for parts of the hand (specifically, the fourth and fifth fingers, the palm, and the inside portion of the forearm.)
The ulnar nerve can be compressed as it passes through the elbow or wrist. However, the elbow is the most vulnerable point because the ulnar nerve is near the surface and travels through a small space (called the cubital tunnel) within the elbow. The ulnar nerve is surrounded by a ligament that (under certain conditions) can thicken and compress the nerve. It is the excessive pressure on the nerve causes symptoms.
What are the Causes of Ulnar Nerve Entrapment?
Things that can contribute to the development of cubital/ulnar tunnel syndrome include:
- Prolonged, repetitive use of the arm or elbow (including leaning on the elbow).
- Elbow injuries: Any trauma (fractures, dislocations or sprains) can cause swelling or compression.
- Medical conditions that can lead to nerve damage (like arthritis and diabetes).
- Abnormal growths: Development of a tumor or cyst that presses against the nerve.
- In some people, the nerve moves back and forth as the elbow is bent and straightened. Over time, this back and forth movement can irritate the nerve.
- Conditions that cause long-term swelling or inflammation near the nerve.
- Long-term pressure on the base of the palm.
- Pregnancy: Hormonal changes can lead to fluid retention. Here, the symptoms typically go away after delivery.
- Sex: Women are more likely to develop ulnar tunnel syndrome than men.
Although there are many known factors that can contribute to the development of cubital/ulnar tunnel syndrome, there are cases where no cause can be identified.
Symptoms of Ulnar Nerve Entrapment
Often symptoms develop gradually and may only include weakness initially. As the syndrome progresses, it may become more difficult do during certain tasks with the hands.
Symptoms of ulnar nerve damage (neuropathy) may include:
- Hand weakness (especially of the little finger and hand grip).
- Numbness, tingling or decreased sensation in the palm or last two fingers. This may be worse at night while sleeping.
- Pain (which can manifest itself as a burning sensation) in the elbow, palm and/or last two fingers. Activities that use the arm may increase the pain.
- Tenderness in the elbow joint at the "funny" bone.
- Loss of finger dexterity (coordination).
- Sensitivity to cold (i.e., symptoms are made worse by cold).
Diagnosis of Ulnar Nerve Entrapment
A physician may perform following to diagnosis cubital/ulnar tunnel syndrome:
- Medical history: Discussing medical history (including prior elbow injuries), current symptoms, and the activities you do (or have done) with your arm/elbow and their frequency.
- Physical examination: Looking for tenderness and/or swelling of the elbow or base of the palm. Checking the muscle strength of the hand, fingers and arm. Pressing or tapping on the elbow (i.e., on the ulnar nerve) to see what sensations occur.
- Laboratory tests: To determine if there any medical conditions (e.g., diabetes).
- Imaging studies: X-rays can help identify things such as arthritis or a fracture. Ultrasound can reveal if there is impaired movement of the ulnar nerve. Occasionally, computed tomography (CT) or magnetic resonance imaging (MRI) may be used to see the anatomy of the elbow or wrist; they can also reveal if there is a tumor or cyst pressing on the nerve.
- Electrophysiological tests: Nerve conduction study and/or an electromyography (EMG). These test the function of the ulnar nerve and can also reveal any other nerve dysfunction that may be present.
Treatment Options for Ulnar Nerve Entrapment
Underlying medical conditions (e.g., arthritis or diabetes) contributing to cubital/ulnar tunnel syndrome should be treated first. Resting the affected elbow and hand for a period of time, changing patterns of arm use and avoiding activities that aggravate the symptoms may be helpful.
A splint or brace to keep the elbow and/or wrist in a straight position may reduce pressure on the nerve. A brace can be worn during activities that aggravate symptoms or at night. Putting an ice pack on the elbow and/or wrist can reduce swelling. Physical therapy that includes stretching and strengthening exercises may be helpful. Medications (both prescription and nonprescription) can be used to temporarily decrease inflammation and ease pain. Treatment can also include a corticosteroid injection into the cubital tunnel to reduce swelling and pressure on the nerve.
If symptoms are severe or do not improve after a few months, surgery may be needed. The goal of surgery is to decompress the ulnar nerve (i.e., remove the pressure on it). Decompression may involve relocation of the nerve. Most of the surgeries can be done on an outpatient basis. If the ulnar nerve is compressed or irritated due to a cyst, tumor, or scar tissue these must be removed.
Three main procedures can be done when the nerve is compressed at the elbow:
- Cubital tunnel release: This is similar to the carpal tunnel release procedure. To enlarge the space within the cubital tunnel, a ligament that makes up part of it is cut, and tissue around the nerve may be removed. Following the procedure, the ligament will begin to heal in a way that provides more room in the cubital tunnel. This procedure does not work well if a patient's ulnar nerve moves back and forth as the elbow is bent and straightened.
- Ulnar nerve transposition: Here the ulnar nerve is permanently moved to new location in the elbow. This procedure prevents the nerve from moving back and forth and stretching as the elbow is bent and straightened.
- Medial epicondylectomy: Here part of a bone in the elbow (the medial epicondyle) is removed. This procedure also prevents the nerve from moving back and forth and stretching as the elbow is bent and straightened.
After surgery, patients may be required to wear a brace/splint for a period of time. The first few days after surgery, the arm should be elevated frequently. To reduce swelling and stiffness patients may be instructed to move their fingers, as well as apply an ice pack. Minor soreness around the incision is common and may last for several weeks. Symptoms may be relieved immediately; however, a full recovery can take several months. The length of recovery depends on how badly damaged the ulnar nerve is. Although the majority of patients recover completely, in severe cases some symptoms will decrease but may not completely go away.
The surgeon will determine what postoperative restrictions are necessary and the estimated time required before a patient can return to work. Patients will be required to undergo a period of physical therapy to restore strength and flexibility.








